What is IVF-ICSI?
ICSI stands for intracytoplasmic sperm injection. IVF ICSI is a technique used as part of a fertility treatment and therefore corresponds to in vitro fertilisation with intracytoplasmic microinjection of a sperm cell. In other words, a sperm cell is injected directly into the oocyte.
The first ICSI was performed at the Centre for Reproductive Medicine of the Free Dutch-speaking University of Brussels. The first French birth by IVF ICSI took place in 1994 at the American Hospital in Neuilly-sur-Seine (Hauts-de-Seine).
In 2017, IVF-ICSI was the second most frequently used technique of ART (Assisted Reproductive Technologies).
What are the differences between IVF-ICSI and conventional IVF?
'Classic' IVF
During conventional IVF, sperm cells are placed directly in contact with an oocyte. Fertilisation therefore takes place spontaneously, but "in vitro", i.e. in the laboratory.
50,000 sperm / oocyte
VS
IVF-ICSI
In IVF-ICSI, a single sperm cell is selected on morphological criteria. It is then placed directly into the oocyte to maximise the chances of fertilisation.
During IVF ICSI, only 1 sperm cell is injected into the oocyte.
IVF ICSI, a solution for male infertility
In vitro fertilisation ICSI requires just one sperm cell to produce an embryo.
This intracytoplasmic sperm injection technique is therefore particularly indicated for male infertility problems in a number of cases:
Asthenospermia (or asthenozoospermia)
Commonly known as "lazy sperm syndrome", this form of male infertility causes an abnormality in the sperm that affects sperm mobility and can compromise natural fertilisation. Following a fertility plan by opting for IVF ICSI can increase the chances of fertilisation in cases of asthenospermia.
Severe oligospermia
In cases of severe oligospermia, where the number of sperm cells collected is very low (less than 1 million sperm per millilitre of semen), IVF ICSI with intracytoplasmic microinjection is particularly indicated. An insufficient sperm count compromises the chances of success of conventional IVF.
Severe teratospermia
A cause of male infertility, severe teratospermia corresponds to a high number of morphological abnormalities in the sperm. It is generally associated with a high rate of DNA fragmentation and chromosomal abnormalities, which are deleterious during fertilisation and embryonic development. In the case of teratospermia, in vitro fertilisation (ICSI) is particularly effective, as the selected sperm is injected directly into the oocyte, thereby compensating for the morphological abnormalities that prevent fertilisation.
In cases of illness
If the male partner has an infectious disease (HIV, hepatitis B or hepatitis C), IVF ICSI can limit the risk of transmitting the infection to the woman. In addition, after cancer treatment with chemotherapy, frozen biological samples are so valuable that ICSI IVF is recommended.
What is the IVF ICSI protocol?
Apart from the in vitro fertilisation process, which differs, the ICSI IVF procedure is very similar to that of conventional IVF. It begins with ovarian stimulation in the woman to stimulate the growth of as many oocytes as possible. These are retrieved by egg retrieval. At the same time, the sperm is collected. Oocytes and the sperm cells are ready: the fertilisation process using intracytoplasmic sperm injection (IVF ICSI) can then take place.
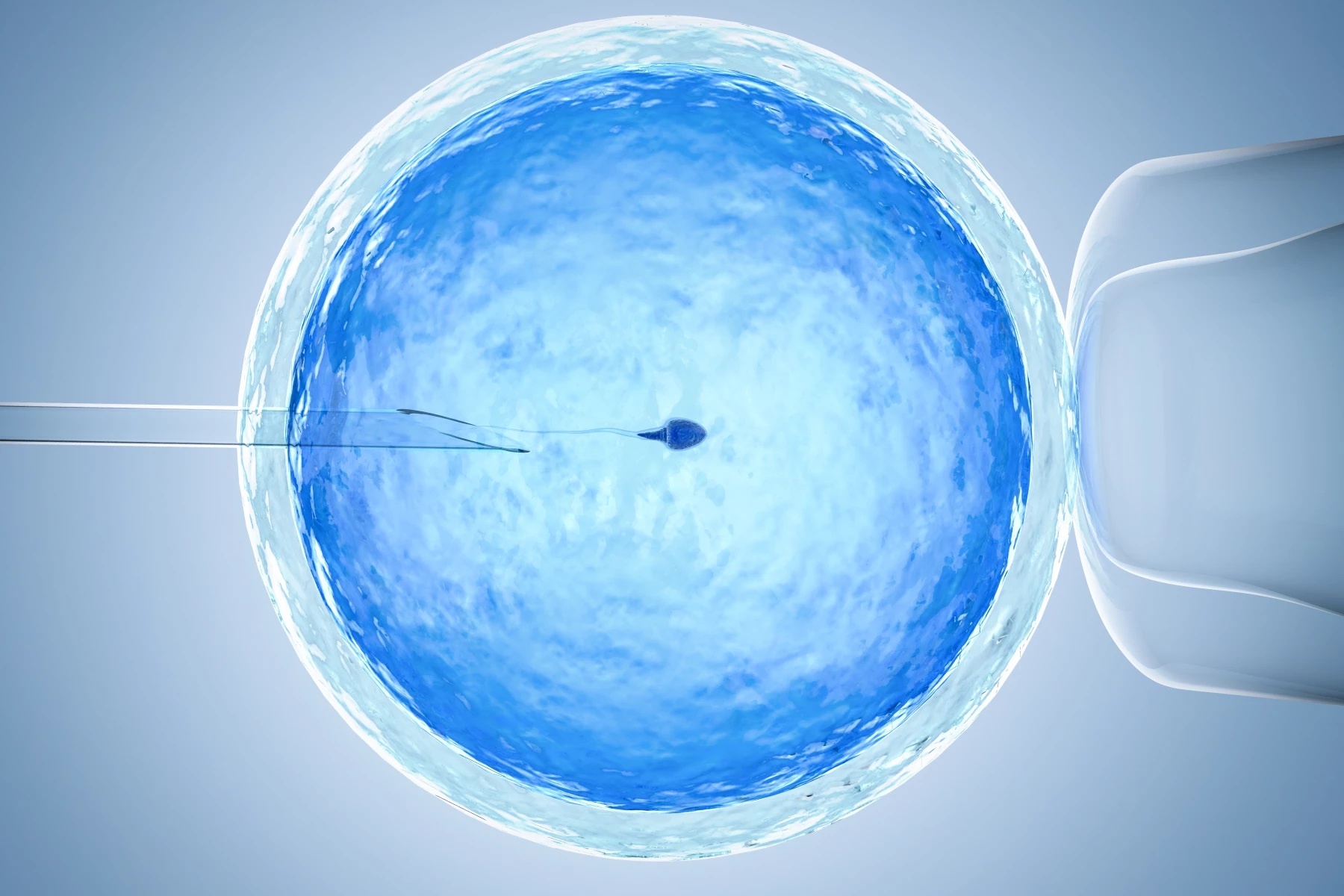
During IVF ICSI, in vitro fertilisation is carried out under a microscope:
A micropipette is used to hold the oocyte by suction (on the left of the photo). At the same time, the sperm cell is selected and aspirated into the injection pipette (on the right of the photo). This selection is based on morphological and mobility criteria. It is then reinjected into the oocyte. Signs of fertilisation and embryonic development are observed the following day with a view to transfer.
IVF ICSI: success rate?
In 2017, according to the Biomedicine Agency's medical and scientific report, 7,863 births were achieved following 43,254 ICSI IVF attempts. The IVF ICSI success rate (number of births per number of attempts) is therefore 18.1%.
A study carried out in the United Kingdom showed that ICSI IVF increased in vitro fertilisation rates compared with conventional IVF (82.7% vs. 67.0%).
IVF ICSI is the in vitro fertilisation technique that offers the greatest chance of success during a fertility treatment.
Written by:
Fabien Duval, Ph.D
Reproductive and developmental biology
Wistim